අනාරක්ෂිත ලිංගික සබඳතා නිසා ඇති වන "ගැබ්ගෙල පිළිකා"
මානව පැපිලෝමා වෛරසය ( Human Papilloma Virus ) ආසාදනය වීම හේතුවෙන් කාන්තාවන්ට ගැබ්ගෙල පිළිකා තත්වය ඇති විය හැකි ය. ලෝක සෞඛ්යය සංවිධානය ඇස්තමේන්තු කර ඇති පරිදි ලොව පුරා කාන්තාවන් 570,000 ක් දෙනා ගැබ්ගෙල පිළිකාවෙන් පෙළෙන අතර එම හේතුවෙන් මේ වන විට කාන්තාවන් 311,000 පමණ මිය ගොස් ඇත.
මෙම මානව පැපිලෝමා වෛරසය අධි අවධානම් වෛරසයක් වන අතර එම වෛරසය දිගින් දිගටම ආසාදනය වීම පිළිකා තත්වයක් කරා ගමන් කරයි. ගැබ්ගෙල පිළිකා රෝගීන් ගෙන් 99% කටම මෙම රෝගය සම්ප්රේෂණය වී ඇත්තේ ලිංගික සබඳතා මුල් කරගෙනයි.
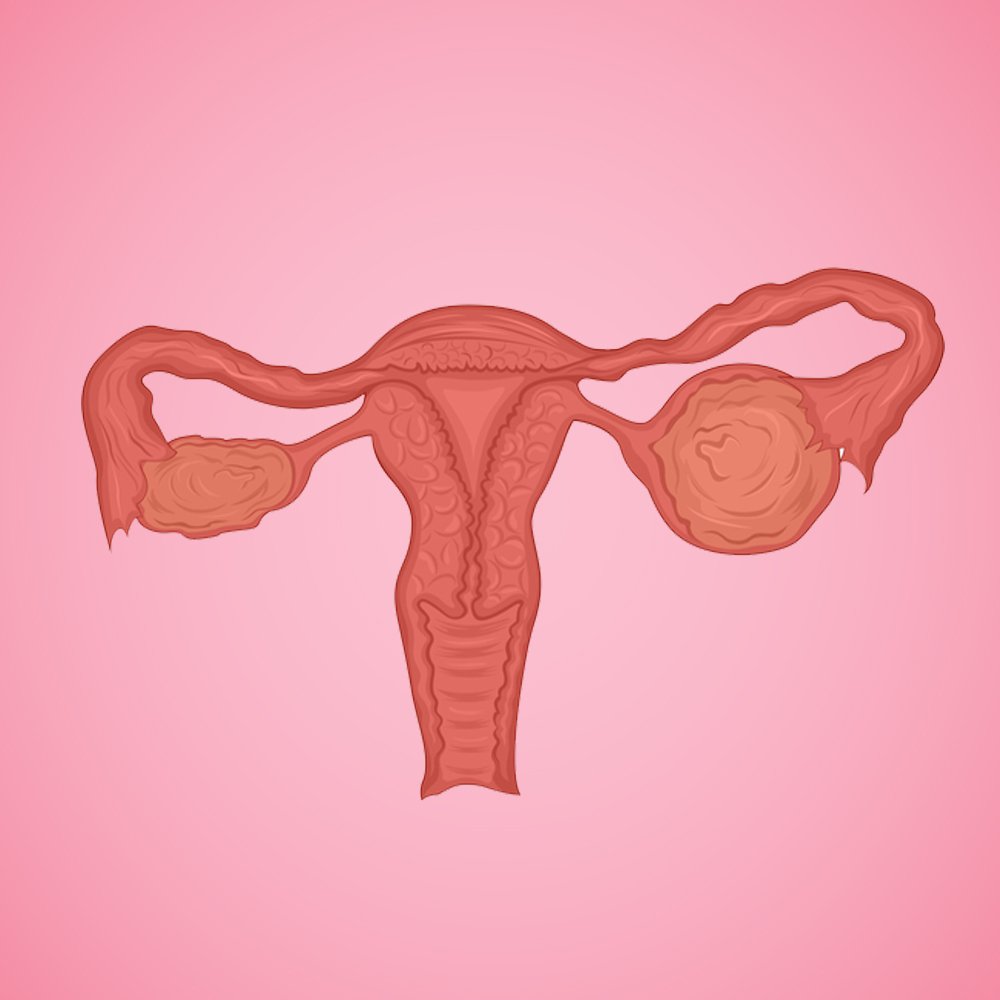
ගර්භාෂයක පහතින්ම පිහිටා ඇති කොටස ගැබ්ගෙල යි. මෙම කොටස සෙන්ටිමීටර දෙකකින් පමණ දිගින් යුක්ත වෙයි. එය යෝනි මාර්ගය හරහා ගර්භාෂයේ ඉහළ කොටසට සම්බන්ධ වන තැන ලෙස හැඳින්විය හැකි ය. ලිංගික සංසර්ගයේ දී එක් පුද්ගලයෙකුගෙන් තවත් පුද්ගලයෙකුට මානව පැපිලෝමා වෛරසය ආසාදනය වන නමුත් කාන්තාවන් ස්වල්ප දෙනෙකුට ගැබ්ගෙල පිළිකා ඇතිවීමේ අවදානම පෙන්වයි.
ලෝක සෞඛ්යය සංවිධානය දක්වන ආකාරයට 2018 වර්ෂයේදී සිදු වූ ගැබ්ගෙල පිළිකා මරණවලින් 90% කට ආසන්න ප්රමාණයක් සිදු වී ඇත්තේ අඩු හා මධ්ය ආදායම් ලබන රටවල්වල යි. 2018 මැයි මාසයේ දී ලෝක සෞඛ්යය සංවිධානයේ අධ්යක්ෂ ජෙනරාල්වරයා ගැබ්ගෙල පිළිකාව තුරන් කිරීම සඳහා ගෝලීය කැඳවීමක් නිකුත් කරන ලදී. එමගින් සියලුදෙනා මෙම ගැබ්ගෙල පිළිකා මර්දනයට සහය විය යුතු බවට අවධාරණය කර ඇත. එහි ප්රතිථලයක් වශයෙන් 2020 අගෝස්තු මාසයේ දී ලෝක සෞඛ්යය සංවිධානය ගැබ්ගෙල පිළිකා තුරන් කිරීමේ ගෝලීය උපාය මාර්ගය සම්මත කළේය.
ගැබ්ගෙල පිළිකා ඇතිවීමට හේතු මොනවාද?
- පළමු ගැබ් ගැනීම අඩු වයසින් සිදුවීම
- පළමු ලිංගික එක්වීම අඩු වයසින් සිදු වීම ( වයස 16 ට අඩුවෙන් )
- ඉතාමත් දිගු කාලයක් උපත් පාලන පෙති භාවිත කිරීම
- කාන්තාවන් මත්ද්රව්ය සහ මත්පැන් අධික ලෙස භාවිත කිරීම
- ලිංගාශ්රිතව සම්ප්රේෂණය වන රෝගවලින් පීඩා විඳීම ( Sexual Transmitted Diseases )
- ලිංගික සහකරුවන් හෝ සහකාරියන් විශාල ප්රමාණයක් ඇසුරු කිරීම
- දරු උපත් වාර ගණන වැඩි වීමත් සමග දරු උපත් අතර පරතරය අවම වීම
ලෝක සෞඛ්යය සංවිධානයට අනුව ගැබ්ගෙල පිළිකාව කල් තියා හඳුනා ගැනීමෙන් ඉතා සාර්ථකව සුව කළ හැකි රෝග විශේෂයකි. ඇතැම්විට ගැබ්ගෙල පිළිකාව ප්රමාද වී හඳුනාගත්ත ද එයට සුදුසු රසායනික සහ විකිරණ චිකිත්සාවන් මගින් සුව කළ හැකිය. 2018 වර්ෂයේ දී ගැබ්ගෙල පිළිකා පැවති ප්රධාන රටවල් 20 අතරින් ‘අප්රිකාව’ ඉහල අගයක් ගන්නා ලදි යි. එසේම ලෝකයේ දුප්පත් රටවල ජීවත්වන කාන්තාවන් අතරින් ගැබ්ගෙල පිළිකා පවතින කාන්තාවන් දස දෙනෙකුගෙන් නව දෙනෙකුම මෙම රෝගය නිසා මරණයට පත් වෙයි.
ගැබ්ගෙල පිළිකාව කල්තියා හඳුනාගත හැකි ලක්ෂණ
- යටි බඩ ආශ්රිත වේදනාව
- ඉතාමත් දුර්ගන්ධයකින් යුතු යෝනි ශ්රාවයන් පිට වීම
- ලිංගික එක්වීමක් අතරතුර සහ ලිංගික එක්වීමකින් අනතුරුව සිදුවන රුධිර වහනය
- මුත්රා මාර්ගය සහ ඒ අවට සිදුවන රුධිර වහනය
- මුත්රා පිට වීමේ වාර ගණන වැඩි වීම
- මලපහ සමග රුධිරය පිට වීම
- ගුඳ මාර්ගය ආශ්රිතව ඇතිවන වේදනාව
- ශරීරයේ බර අසාමාන්යය ලෙස පහත වැටීම
- ශරීරය සුදුමැලි වීම
- නිතර ඇතිවන තෙහෙට්ටුව
ගැබ්ගෙල පිළිකාව වළක්වා ගන්නේ කෙසේද?
- වයස අවුරුදු 15 දී වත් HPV ( මානව පැපිලෝමා වෛරසය) එන්නත ලබා ගැනීමට යොමු වීම
- ලිංගික සහ ප්රජනක සෞඛ්යය පිලිබඳව දරුවන්ව නිසි වයසේ දී දැනුවත් කිරීම
- අනාරක්ෂිත ලිංගික හැසිරීම් නැවැත්වීමට කටයුතු කිරීම
- යොවුන්වියේ ගැහැනු ළමුන් සහ පිරිමි ළමුන් සෞඛ්යය සම්පන්න ජීවන රටාවන්ට යොමු කිරීම
- ලිංගික සහකරුවන් ප්රමාණය සීමා කිරීම
- ලිංගික සබඳතාවල දී කොන්ඩම් වැනි ආරක්ෂිත ක්රම භාවිත කිරීම
- බොහෝ ලිංගික සහකරුවන් හෝ සහකාරියන් ප්රමාණයක් ඇසුරු කරන පුද්ගලයන් සමග ලිංගික සබඳතා නැවැත්වීම
- ලිංගික ඉන්නන් හෝ වෙනත් ලිංගාශ්රිත රෝග ලක්ෂණ පෙන්නුම් කරන පුද්ගලයන් සමග ලිංගික සබඳතාවලින් වැළකී සිටීම
- කාන්තාවන් අවුරුදු 35 පසු වන විට පැප් පරීක්ෂණය ( Pap Test ) සිදු කිරීම සඳහා වසර 5 කට වරක් කාන්තා සායනවලට යොමු වීම
- රෝගී තත්වයන් හඳුනා ගත් විගස ප්රතිකාර සඳහා යොමු වීම
එසේම දිනපතා සිය ආහාර වේල සඳහා එකතු කර ගන්නා දේවල් මගින් මෙම පිළිකා තත්වයට එරෙහි ප්රතිශක්තිකරණයක් ශරීරය තුළ ක්රියාත්මක කරයි. නිදසුනක් ලෙස බතල, ගස්ලබු, දොඩම්, තක්කාලි සහ දිනපතා කාබනික එළවළු සහ පලතුරු ආහාරයට ගැනීම, රටකජු, මුංඇට, කළු කවුපි මෙන් ම ඔලිවු තෙල්, මාළු වැනි ආහාර ප්රතිශක්තිකරණ පද්ධතිය ශක්තිමත් කරයි.
අවසාන වශයෙන් අප සිහි තබා ගත යුත්තේ අපගේ ශරීරය අපගේ සියලුම හැඟීම් පිනවීමට භාවිත කිරීමේ ඇති භයානක බවයි. සෑම සබඳතාවක්ම ඉතා ආරක්ෂාකාරීව මෙන් ම වඩාත් ගෞරවාන්විතව සිදු කිරීමට යොමු වන්න. අනාගතයේ ඇති විය හැකි අනතුරු අවම කර ගැනීමට ඔබ වෙනුවෙන් ඔබගේ දායකත්වය ලබා දෙන්න.
ආශ්රිත ග්රන්ථ නාමාවලිය
- Cervical Cancer Elimination Initiative Knowledge Respository, WHO
- Global Cancer Observatory: Burden of Cervical Cancer by country , WHO
- Global Health Observatory data: Death rate for Noncommunicable Diseases ( NCDs)
- Data Portal on Global Statergy for Women’s Children’s and Adolescent’s Health ( 2016 – 2030 ), WHO
- WHO Guideline for screening and treatment of cervical Pre – Cancer lessons for cervical cancer prevention, second edition, WHO
- Implementation of Post – market surveillance in Cervical Cancer Programmes, WHO
- Cervical Cancer, Basic information, CDC, USA.gov
- කුමක්ද? මේ ගැබ්ගෙල පිළිකාව නොහොත් Carcinoma of Carvix? mydoctor.lk, DR.H. Vithana ( M.B.B.S)
Similar Articles...

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of

All you need to know about Gestational Diabetes
Did you know that gestational diabetes mellitus, also known as GMD, is one of the most common medical complications of pregnancy? What is GMD? Why
Endometriosis
Endometriosis No woman looks forward to “that time of the month.” Dealing with nausea, stomach cramps, mood swings, back pains and fatigue, all whilst facing