Cervical Cancer: What You Need To Know
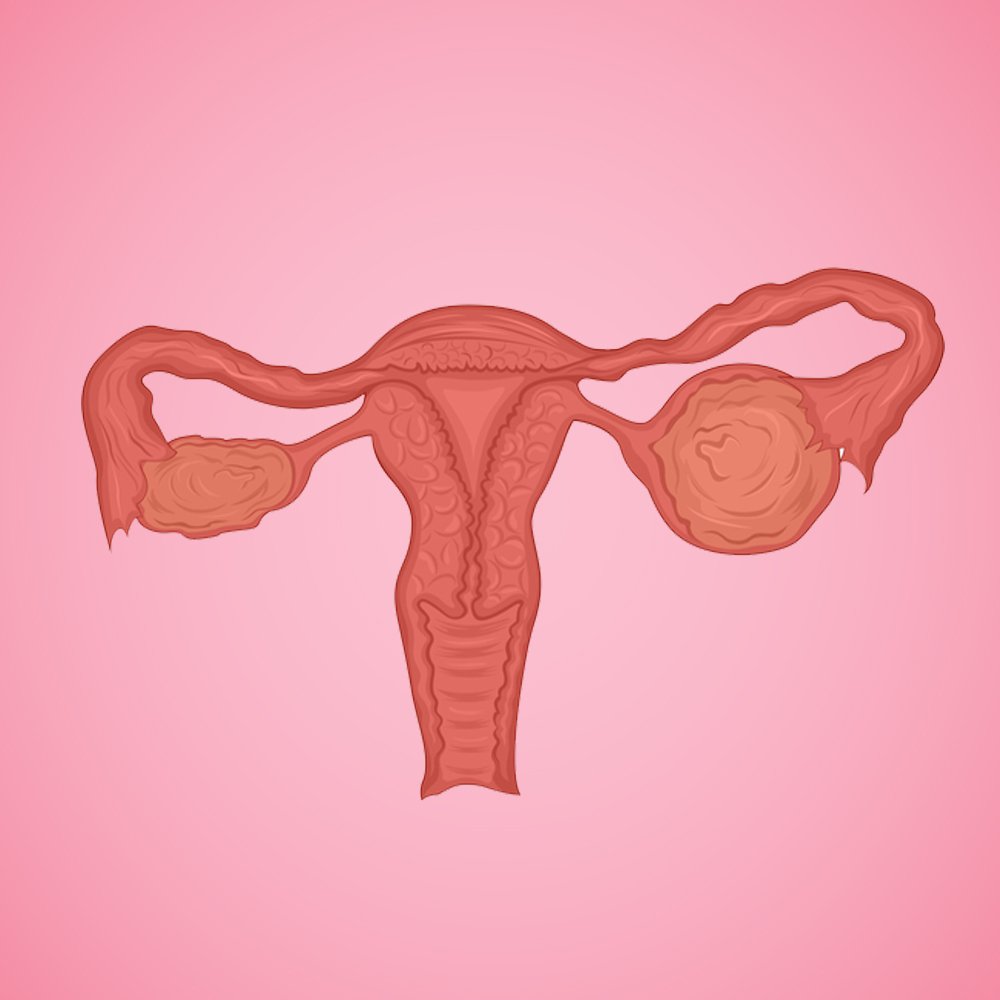
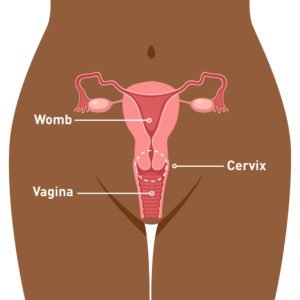
Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the womb that connects to the vagina. Ladies, here’s what you need to know. Gentlemen, don’t scroll past this, if you have women in your life that you care about, here’s what YOU need to know!
Even though this might not be a topic to casually slip into conversation with friends or family members, it is important to know the causes, symptoms, risk factors and preventative measures both men and women have to take when it comes to cervical cancer.
What are the best ways to prevent cervical cancer?
- Pap smears – One of the easiest ways to prevent cervical cancer is by getting screened regularly by your gynecologist who will conduct routine pap smears. Screening picks up precancerous cells, so they can be treated before they turn into cancer. If you are over the age of 25, It’s highly recommended to do annual check-ups with your gynecologist, where pap smears can be done every 5 years.
- HPV vaccination – Currently, the HPV vaccine is given to children along with all their other jabs. For those of you who did not receive the HPV vaccine and if you’re under the age of 25, we recommend getting vaccinated, regardless of your gender and help prevent cervical cancer!
- Limit the number of sexual partners you have.
- Practice safe sex – Always use a condom or other barrier method when you have vaginal, oral, or anal sex.
- Don’t smoke – Smoking is associated with a certain type of cervical cancer, called squamous cervical cell cancer.
Ladies, if you’re sexually active, it’s important to speak to a doctor about pap smears and the HPV vaccine. You don’t need to be nervous to broach the topic as these conversations only help you live your best, healthy life!
What causes cervical cancer?
Various strains of the human papillomavirus (HPV), a sexually transmitted infection, play a role in causing cervical cancers. There are about a 100 strains of HPV and only a few types cause cervical cancer. Being infected with a cancer-causing strain of HPV doesn’t mean you’ll get cervical cancer. Your immune system eliminates the vast majority of HPV infections, often within two years.
HPV is a very common infection. Read more about HPV in our blog here.
In a small percentage of people, however, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
Symptoms of cervical cancer
The early stages of cervical cancer produces no signs or symptoms which makes it difficult for most women to know that they have the disease. When symptoms do appear, they’re easily mistaken for common conditions like menstrual periods and (UTIs).
Typical cervical cancer symptoms are:
- Unusual bleeding, such as bleeding in between periods, after sex, or after menopause
- Vaginal discharge that looks or smells different than usual
- Pain in the pelvis
- The need to urinate more often
- Pain during urination
What factors increase the risk of getting cervical cancer?
HPV is the biggest risk for cervical cancer but other factors include:
- Sex with many different partners, who themselves have many sexual partners can increase the chances of getting HPV.
- Having other STIs — such as chlamydia, gonorrhea, syphilis and HIV/AIDS
- Smoking
- Early sexual activity – Having sex at a younger age can increase your risk of contracting HPV
- Taking birth control pills
- An unhealthy diet
How does a doctor diagnose cervical cancer?
A pap smear is a test doctors use to diagnose cervical cancer. To perform this test, your doctor collects a sample of cells from the surface of your cervix. These cells are then sent to a lab to be tested for precancerous or cancerous changes. Cells which contain HPV can remain in the body for a long time, which is why with regular pap smears every 3 years, doctors can detect precancerous cells and remove them in a painless procedure – preventing those cells from becoming cancerous.
Consult a gynecologist on the oDoc app today to find out more.
References:
- Cervical Cancer, Mayo Clinic (2021)
- Everything You Need to Know About Cervical Cancer, Healthline (2019)
Similar Articles...

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of

All you need to know about Gestational Diabetes
Did you know that gestational diabetes mellitus, also known as GMD, is one of the most common medical complications of pregnancy? What is GMD? Why
Endometriosis
Endometriosis No woman looks forward to “that time of the month.” Dealing with nausea, stomach cramps, mood swings, back pains and fatigue, all whilst facing