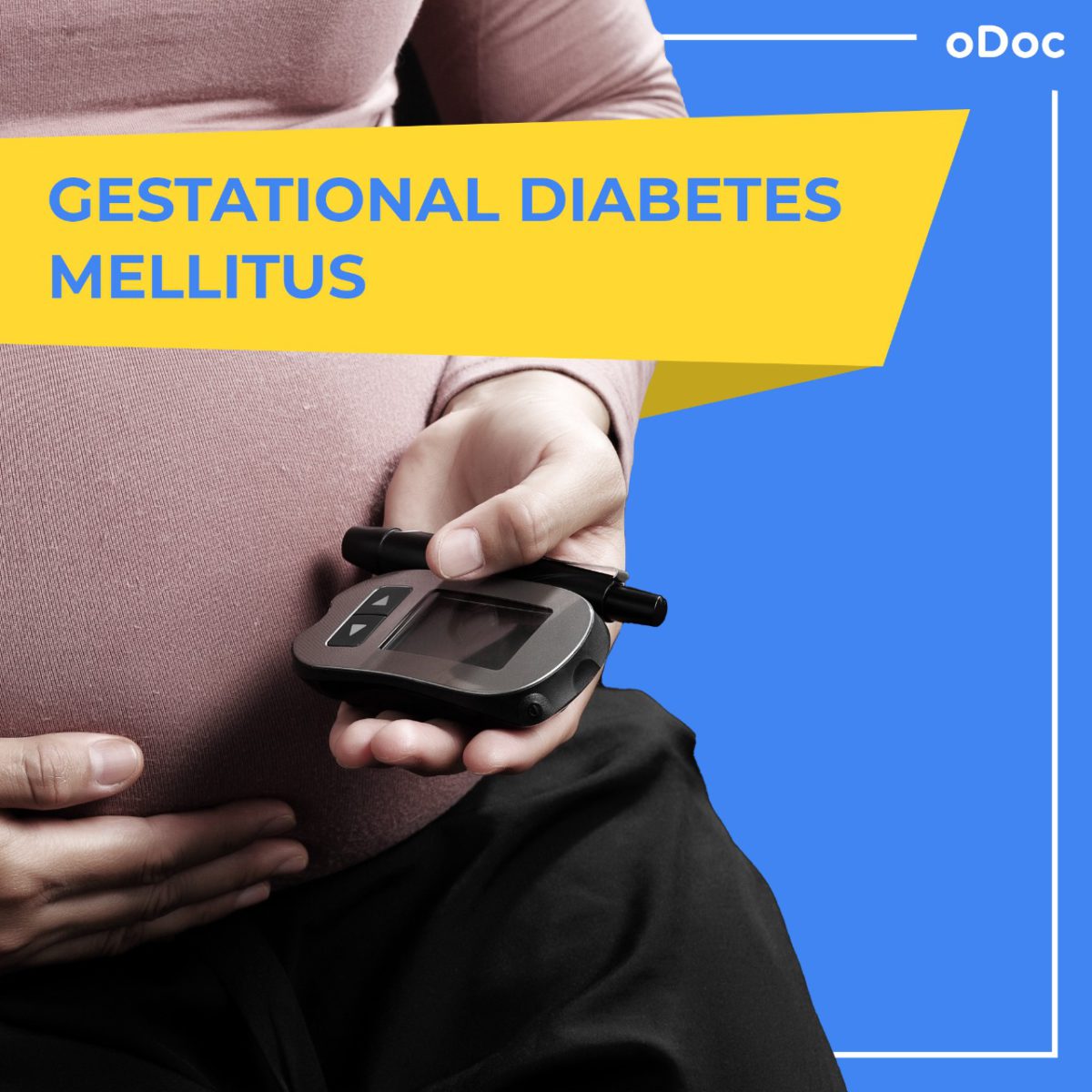
All you need to know about Gestational Diabetes
Did you know that gestational diabetes mellitus, also known as GMD, is one of the most common medical complications of pregnancy?
What is GMD? Why does it happen? Can you prevent it? Keep scrolling for answers.
So, let’s start with the basics. What is gestational diabetes?
Gestational diabetes is high blood sugar that develops during pregnancy and usually disappears after giving birth. Many hormones are involved in maintaining the blood sugar level. As the hormone levels fluctuate during pregnancy, they prevent the body from using insulin effectively, leading to insulin resistance. This causes glucose build-up in the blood instead of being absorbed by the cells. Typically, the pancreas can make additional insulin to overcome insulin resistance, but when insulin production is not enough to overcome the effect of the placental hormones, gestational diabetes results.
A study conducted by Kai Wei Lee et., found the prevalence of GDM in Asia was 11.5%. GMD can happen at any stage of pregnancy but is more common in the second or third trimester.
But why is that?
Scientists have not been able to identify the exact hormone that causes GDM in pregnant women. But, many scientific theories suggest that as the placenta grows, more and more hormones are released, which increases risk of insulin resistance. Thus, symptoms of GMD are seen more often in the 2nd and 3rd trimesters.
What are the symptoms of GMD?
Many women who have GMD do not show symptoms, but the most common ones are:
- Increased thirst
- Urgency to pee more often
- Dry mouth
- Tiredness
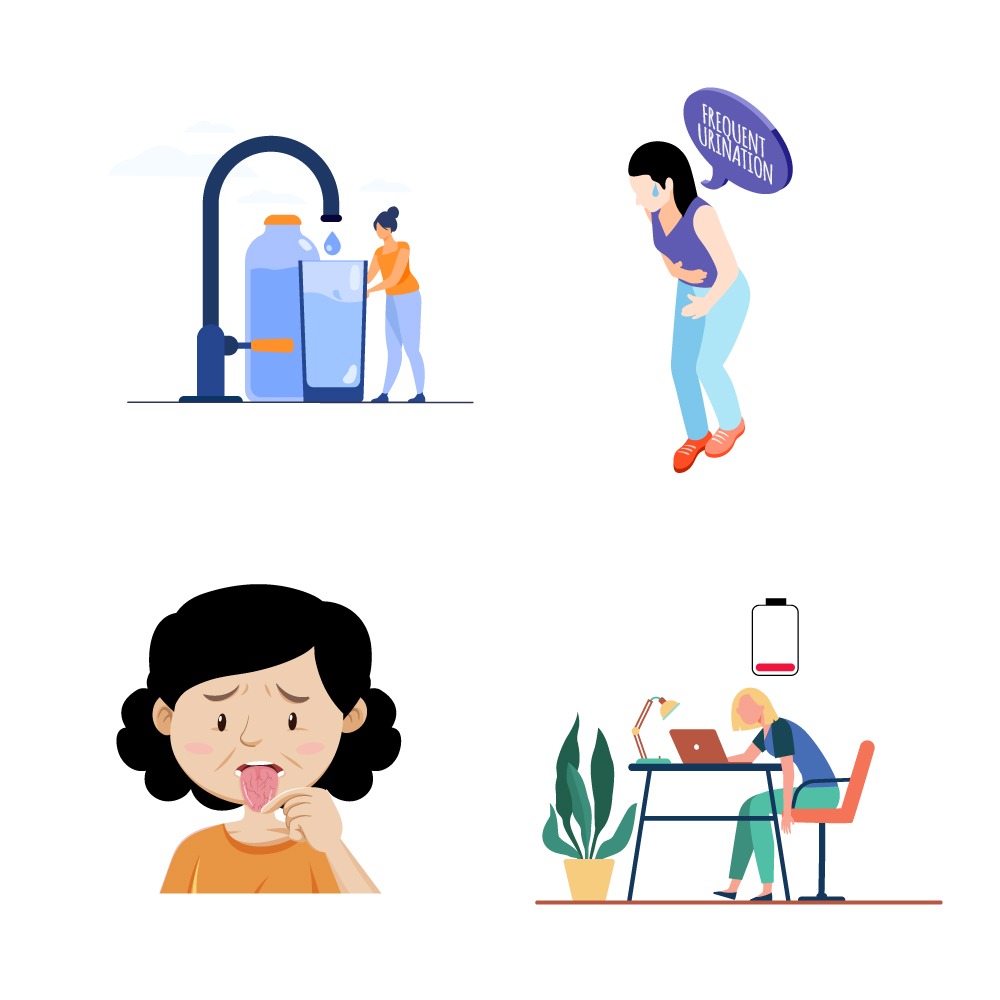
These symptoms are relatively common during pregnancy and not necessarily a sign of GMD. If you are pregnant and have noticed these symptoms, you should speak to a VOG doctor or a general physician, via oDoc who will provide a prescription for a lab test. You can carry out the lab tests from the comfort of you home via oLabs too.
Who is at risk?
GMD can affect any woman, but a list of risk factors identified by scientists increases the chances of developing GMD.
The risk factors include
- Being overweight before pregnancy
- Having a family history of diabetes
- Being Prediabetic (if you have a blood glucose level higher than normal but not high enough to be classed as diabetic.
- Having PCOS
- Being older than 25 as they are at a greater risk for developing gestational diabetes than younger women
- Having high blood pressure, high cholesterol, heart disease, or other medical complications
- Having given birth to a large baby (weighing more than 9 pounds)
- Having had a miscarriage
How does GMD affect the mother and the baby?
More often than not, women who have GMD go on to have normal pregnancies and deliver healthy babies. However, in other circumstances, GMD can lead to:
- Macrosomia. This is where the baby grows very large as they absorb the excess glucose in the mother’s blood and convert it into fat and are deposited. This leads to difficulties during labour, causing doctors to opt for induced labour and c-section.
- Too much amniotic fluid (the fluid that surrounds the baby) in the womb can cause premature labour or problems at delivery, known as polyhydramnios.
- Premature birth
- Low blood sugar (hypoglycemia) in the baby after delivery. This happens because the mum’s high blood sugar level also causes the baby to have a high blood sugar level, and after birth, it no longer has the high level of sugar from its mother, resulting in the newborn’s blood sugar level becoming very low.
- Obesity and type 2 diabetes later in life for babies. Babies of mothers with gestational diabetes have a higher risk of developing obesity and type 2 diabetes later in life.
- Stillbirth. Untreated, gestational diabetes can result in a baby’s death before or shortly after birth.
- Future diabetes for the mother. If you have gestational diabetes, you’re more likely to get it again during a future pregnancy. You also have a higher risk of type 2 diabetes as you get older.
What are the treatment options?
The American Diabetes Association recommends screening for undiagnosed type 2 diabetes at the first prenatal visit in women with diabetes risk factors. In pregnant women not known to have diabetes, GDM testing should be performed at 24 to 28 weeks of gestation.
If you are found to have GMD, don’t worry, as it can be treated, and complications can be reduced. The doctor may ask you to monitor your blood sugar level often, exercise often, eat healthily and maybe give insulin injections if necessary.
How is it prevented?
There are no guarantees for preventing gestational diabetes — but the more healthy habits you can adopt before pregnancy, the better.
So don’t forget to
- Eat healthy – Choose foods high in fibre and low in fat and calories.
- Exercise often – Exercising before and safely during pregnancy can help protect you from developing gestational diabetes.
- Start pregnancy at a healthy weight. If you’re planning to get pregnant, losing extra weight beforehand may help you have a healthier pregnancy.
If you are pregnant and experiencing any of the symptoms mentioned above or have any questions, you can speak to one of the Obstetricians, Gynaecologists or GPs on the oDoc app. Click here to download the app.
Sources
- Alfadhli, E., 2015. Gestational diabetes mellitus. Saudi Medical Journal, 36(4), pp.399-406.
- Gestational Diabetes Mellitus (GDM). (n.d.). Johns Hopkins Medicine. Retrieved April 6, 2022, from
- Gestational diabetes – Symptoms and causes. (2020, August 26). Mayo Clinic.
- NHS website. (2021, November 29). Gestational diabetes. Nhs.Uk.
- Lee, K.W., Ching, S.M., Ramachandran, V. et al. Prevalence and risk factors of gestational diabetes mellitus in Asia: a systematic review and meta-analysis. BMC Pregnancy Childbirth 18, 494 (2018).

Similar Articles...

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of

All you need to know about Gestational Diabetes
Did you know that gestational diabetes mellitus, also known as GMD, is one of the most common medical complications of pregnancy? What is GMD? Why
Endometriosis
Endometriosis No woman looks forward to “that time of the month.” Dealing with nausea, stomach cramps, mood swings, back pains and fatigue, all whilst facing