Your Skin is Your Superhero: The Power of Skincare for Glowing and Healthy Skin
Our skin is not just a protective layer; it is a superhero that safeguards us from external threats and keeps our body functioning optimally. As the largest organ and the most significant muscle in the human body, our skin deserves our utmost care and attention. In this article, we will explore the importance of skincare, particularly for dry skin, and discover how to unlock the superpowers of your skin for a radiant and glowing complexion.
Understanding Skincare: More than Meets the Eye
Skincare is not just about applying creams and lotions; it is a holistic approach to nourishing and protecting our skin. Our skin acts as a barrier, shielding us from harmful UV rays, bacteria, pollution, and other environmental stressors. It also helps regulate body temperature and maintains moisture balance, crucial for overall skin health.
The Battle Against Dry Skin
Dry skin is a common concern many individuals face, especially during colder months or in dry climates. It can lead to discomfort, itchiness, and a dull complexion. Adopting a skincare routine that replenishes moisture and supports the skin’s natural barrier function is essential to combat dryness.

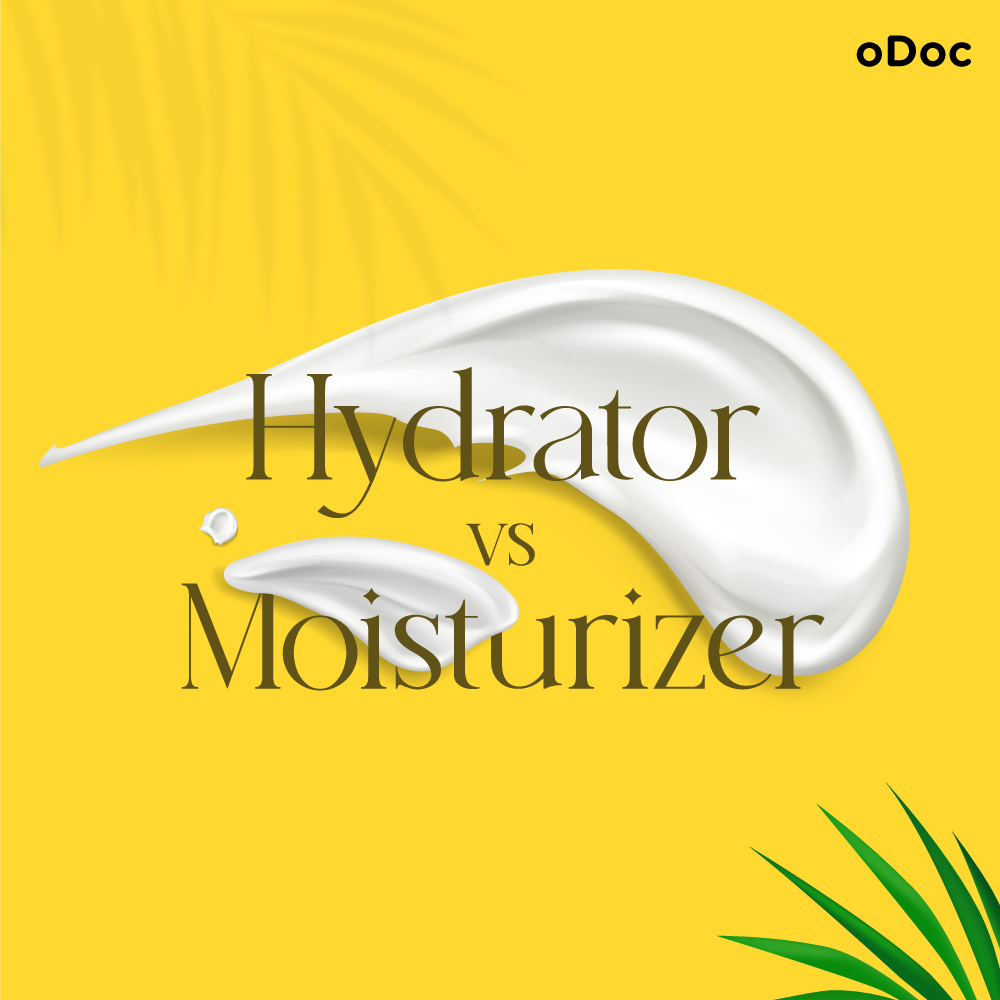
Hydration is Key
The first step towards revitalising dry skin is to ensure adequate hydration. Drink plenty of water throughout the day to keep your body hydrated from within. Additionally, use a hydrating cleanser that doesn’t strip away natural oils and opt for a moisturiser for dry skin. Look for ingredients like hyaluronic acid, glycerin, and ceramides, which help attract and retain moisture, leaving your skin plump and supple.

Exfoliation for Renewal
Exfoliation is a crucial step in any skincare regimen, especially for those with dry skin. By gently removing dead skin cells, you allow fresh, healthier skin to emerge. Opt for a mild chemical exfoliant containing alpha-hydroxy acids (AHAs) or beta-hydroxy acids (BHAs). These gentle acids dissolve the bonds between dead skin cells, revealing a smoother, more radiant complexion.
Note – It is generally recommended to exfoliate dry skin 1-2 times a week to avoid over-exfoliation and irritation.
Protect and Shield your Skin
Protecting your skin from harmful UV rays is vital in maintaining health and preventing premature ageing. Apply a broad-spectrum sunscreen with at least SPF 30 daily, even during cloudy weather. Sunscreens containing antioxidants like vitamin C provide additional protection against free radicals, ensuring your skin stays youthful and glowing.
Superfoods for Super Skin
Just as superheroes need a proper diet to fuel their powers, our skin thrives on a balanced and nutritious intake. Include antioxidant-rich foods, such as berries, leafy greens, and nuts, to promote collagen production and fight free radicals. Omega-3 fatty acids in fatty fish, chia seeds, and walnuts can help maintain skin elasticity and reduce inflammation.

Your skin is indeed your superhero, tirelessly protecting you day in and day out. By investing in a skincare routine that focuses on hydration, exfoliation, and sun protection, you can unleash your skin’s full potential and achieve a glowing, healthy complexion. Remember, your skin’s health reflects your overall well-being, so treat it with the care and attention it deserves. To get more personalised care and guidance on your skin, speak to a dermatologist with just a few taps via oDoc!
Embrace the power of skincare and let your skin shine like the superhero it truly is!
With these practices and a commitment to consistent skincare, you can unlock the superpowers of your skin, allowing it to thrive and reveal its natural radiance. So, embrace the power of skincare, make it a part of your daily routine, and let your skin shine like the superhero it truly is!
Sources
Skin care: 5 tips for healthy skin.” Mayo Clinic, https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/skin-care/art-20048237
How to Take Care of Your Skin.” Healthline, https://www.healthline.com/health/beauty-skin-care/skin-types-care
Similar Articles...

Let’s talk flu, its prevention and home remedies.
Boo-ger season is here! Let’s begin by defining flu (short term for influenza) because it’s usually misunderstood as fever or cold. Flu is a common

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of
How to Keep Work Stress from Taking Over Your Life
How to Keep Work Stress from Taking Over Your Life In today’s fast-paced and competitive world, work stress has become an all-too-common problem that affects