The First Trimester
Happy, anxious, nervous, scared, overjoyed and excited. These are just a few of the emotions you may experience when you first find out you are pregnant. If it is your first time you are definitely going to feel a bit confused and will resort to googling everything related to pregnancy. We have broken down everything you need to know about the first trimester of pregnancy in this blog.
So what is the first trimester of pregnancy?
It is the earliest phase in your pregnancy. It starts on the first day of your last period and ends on the last day of the 13th week. During your first trimester of pregnancy, a lot of changes happen to you and the baby. So keep reading to find out what is in store for you
What are the changes happening in your body?.
Due to the hormones released by the body,, many changes will occur during pregnancy. These changes help prepare you for the 9 months of pregnancy.
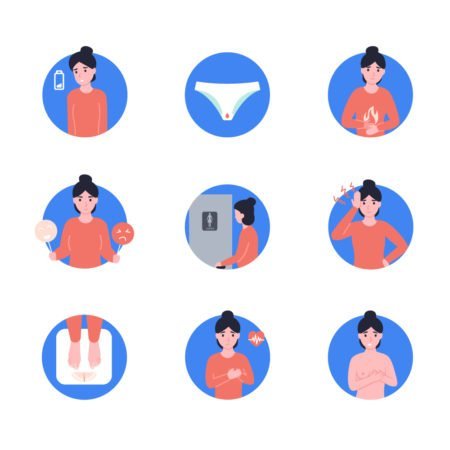
- Swelling of breasts– caused by the mammary glands enlarging to prepare for lactation as a result of increased oestrogen and progesterone hormones secretion.
- Peeing more often – you will start peeing more often as your uterus grows and presses against your bladder.
- Darken and enlarged areolas – this is the pigmented area around your nipple. They may also become covered with small, white bumps called Montgomery’s tubercles (enlarged sweat glands).
- Mood swings – you may begin to experience severe mood swings which is caused by the surge in hormones.
- Morning sickness – occurs due to increased hormone levels that is needed to sustain the pregnancy. Contrary to the name, nausea can occur at anytime of day.
- Constipation – occurs as the growing uterus presses against your rectum and intestines.
- Heartburn and indigestion – the increased levels of progesterone can slow the muscular contractions in our intestines.
- Extreme tiredness – caused as a result of the physical and emotional demands of pregnancy.
- High heart rate- caused by the increased cardiac output to supply enough blood to both you and your baby.
- Slight bleeding – About 25% of pregnant women have slight bleeding during their first trimester of pregnancy. Early in the pregnancy, light spotting may be a sign that the fertilized embryo has implanted in your uterus. If you have severe bleeding please seek medical advice urgently.
- Weight gain – this is due to a 40-50% increase in volume of blood in the body during pregnancy and storage of fat in the body which is later used for milk production.
It is important to note that some symptoms of pregnancy continue for several weeks or months. Others are only experienced for a short time. Some women experience many symptoms, and some experience only a few or none at all. Everyone is different but that’s to be expected -you are unique!
Now lets have a look at the changes your baby will go through.
The most development occurs during the first trimester. During the first 13 weeks, your baby develops from a fertilized egg (embryo) into a fully-formed fetus. All major organs are formed during the first trimester of pregnancy. By the end of the first trimester of pregnancy, the fetus weighs approximately 0.5 to 1 ounce and measures, on average, 3 to 4 inches in length.
Here is what exactly happens:
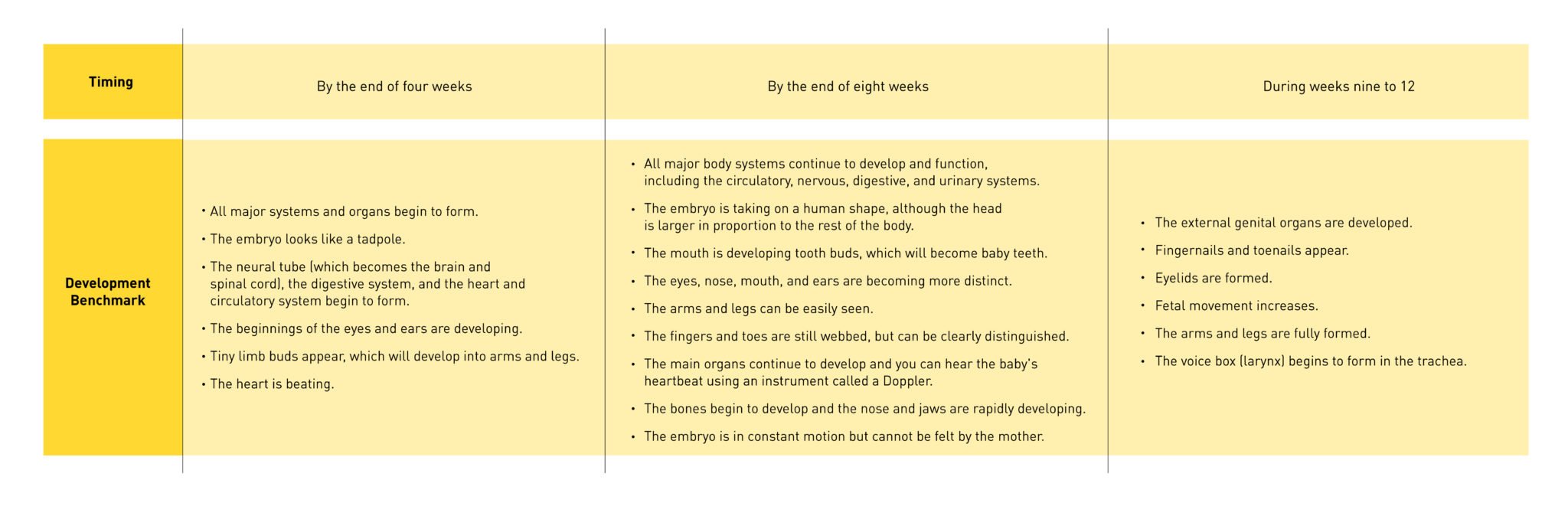
(Source: Johns Hopkins Medicine)
The fetus is most vulnerable during the first 12 weeks. During this period of time, exposure to drugs, radiation, tobacco and other toxic substances can affect the formation of the major organs and body systems.
So what do you need to know while visiting the doctor during the first trimester?
As soon as you find out you are pregnant, make an appointment with your VOG doctor so you can start caring for the baby. You should see your doctor once a month but it is better to discuss this with your VOG doctor.
During your first visit the doctor may:
- perform an ultrasound to confirm the pregnancy
- perform a Pap test
- take your blood pressure
- test for sexually transmitted infections, HIV, and hepatitis
- estimate your date of delivery or “due date,” which is around 266 days from the first day of your last period
- screen for risk factors like anemia
- check thyroid levels
- check your weight
If you experience any of the following please seek medical help immediately:
- Severe abdominal pain
- Heavy bleeding
- Severe dizziness
- Rapid weight gain or too little weight gain
It is also recommended you start building out your birth plan early on during your pregnancy. To know more about how to create your birth plan click here. You can also consult a VOG doctor at any time and from the comfort and safety of your home via the oDoc app.
Source
- Bhargava, H. D. (2020, July 16). First trimester of pregnancy: What to expect, Baby Development. WebMD. Retrieved December 15, 2021, from https://www.webmd.com/baby/guide/first-trimester-of-pregnancy#3
- Healthline Media. (2017, November 9). The first trimester of pregnancy. Healthline. Retrieved December 15, 2021, from https://www.healthline.com/health/pregnancy/first-trimester#other-considerations
- The first trimester. Johns Hopkins Medicine. (n.d.). Retrieved December 15, 2021, from https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-first-trimester
Similar Articles...

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of

All you need to know about Gestational Diabetes
Did you know that gestational diabetes mellitus, also known as GMD, is one of the most common medical complications of pregnancy? What is GMD? Why
Endometriosis
Endometriosis No woman looks forward to “that time of the month.” Dealing with nausea, stomach cramps, mood swings, back pains and fatigue, all whilst facing