We Need To Stop Saying Breastfeeding Is “Easy”
And focus on supporting mothers instead

What if we viewed breastfeeding the same way?
What if instead of glorifying only the ‘highlights reel’ of breastfeeding, we all agree that breastfeeding needs education, preparation and hard work to get through the first few weeks. What if we supported and empowered mothers on this journey filled with sacrifices and challenges and collectively took responsibility for it? What if we celebrated them loudly and genuinely when they achieved their goals?
The recently concluded ‘World Breastfeeding Week’ was triggering for a lot of mothers. For many women, any mention of breastfeeding brings back feelings of pain, anxiety and a lack of support. It serves as a reminder of the guilt and shame that they felt for stopping breastfeeding, the feeling that their bodies weren’t doing what they were meant to do.
Changing the Messaging
A Sri Lankan mum recently told me:
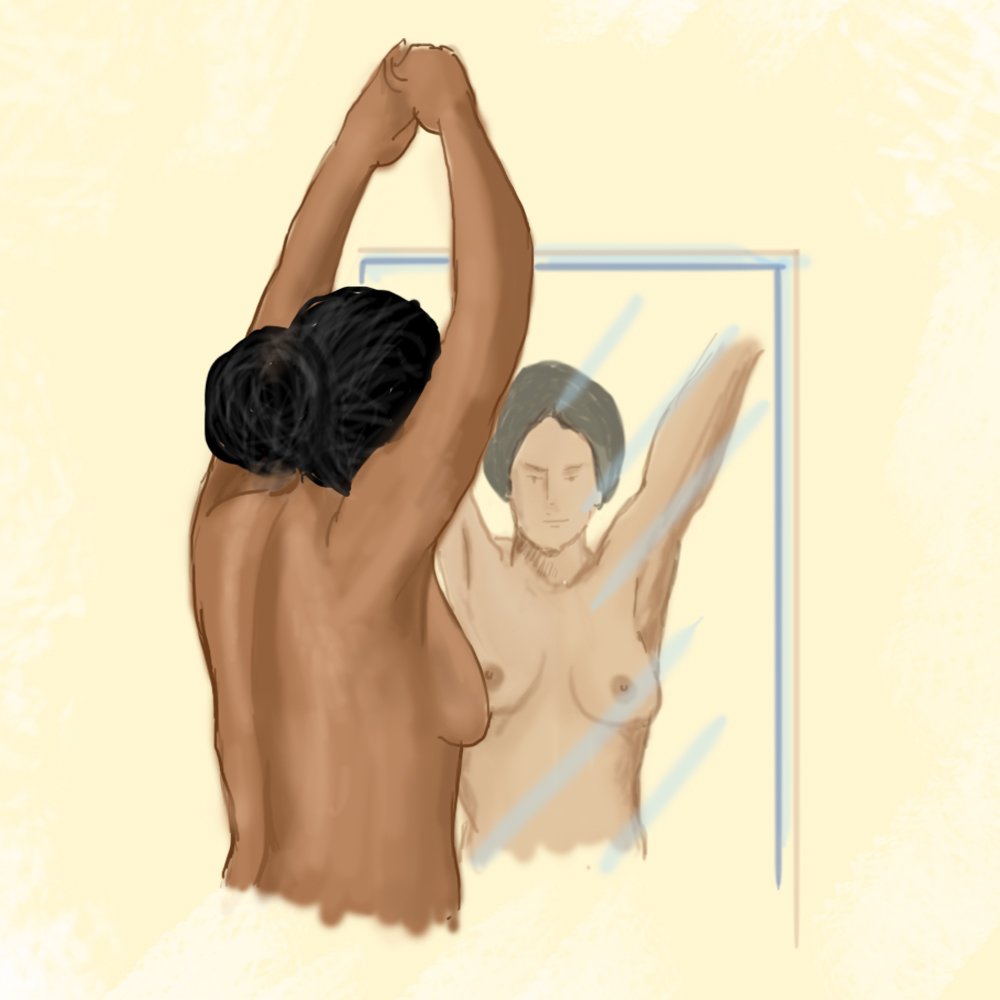
“Breastfeeding is hard… everyone tells you how painful labour is and how difficult pregnancy is, but no one tells you how hard breastfeeding is! All you see are images of moms with babies on their breasts and they make it look like it’s the easiest thing!”
Amy Brown, Professor of Child Public Health, Swansea University says: “When we gloss over the realities of breastfeeding, women feel unprepared for what it’s really like. If we tell women to expect easy, and they hit a hurdle, they may think they’re doing something wrong. . Women then end up depressed, blaming themselves, thinking they didn’t try hard enough because after all, isn’t breastfeeding easy?”
Without swinging towards ONLY the positive or the negative, perhaps the good, the bad and the ugly all need to be portrayed together. We need to find a balance.
So what are the benefits of breastfeeding?
- We sometimes refer to breastmilk as “liquid gold”! Mums often joke that breastmilk is the cure for nearly everything:baby acne, sore eyes, heat rash,eczema and healing our cracked and sore nipples.
- The composition of breastmilk is biochemically and nutritionally complete, giving numerous long term and immunological advantages.. It protects from infections, diarrhoea, UTIs, and chronic diseases like diabetes, childhood cancers, obesity, inflammatory bowel disease, asthma and allergies. In preterm babies, it reduces the risk of sepsis and necrotising enterocolitis (NEC).
- For mothers, it has been proven to reduce the risk of hypercholesterolaemia, diabetes, hypertension, cardiovascular disease, as well as reduce the incidence of breast and ovarian cancer and osteoporosis. It stabilises endometriosis and confers partial contraception.
- The process of breastfeeding stimulates the release of oxytocin, the bonding chemical. Babies don’t only breastfeed to eat, but also to help themselves settle: it provides them comfort and helps them regulate their emotions.
- From a practical standpoint, breastfeeding is free and convenient! No stumbling around in the dark to boil water and prepare a bottle! Your baby has access to fresh milk straight from the source.
OK, I’m convinced of the benefits. Now hit me with the challenges of breastfeeding!
Here in Sri Lanka, we are seeing a rise of an ‘Instagram mum brigade’ who raise awareness on issues surrounding motherhood whilst sharing experiences and building community. They are finding their voices and being the support that they wished they had as new mums.
One of these Instagram mothers, Ameena (IG handle @raisingimaan) – expresses the challenges of breastfeeding so beautifully in a recent post. She said:
“Breastfeeding isn’t simply putting a breast into a baby’s mouth and transferring milk. It is SO MUCH more than that. And women pay for it with a unique currency of time, commitment, energy, mental and physical health, as well as bodily autonomy. That’s a massive price to pay. And to tell women that it’s all on themselves alone to manage. Frankly, it’s quite a raw deal”.

- The first few weeks of breastfeeding, in particular, require a considerable investment of time. It IS time consuming, and new mothers can feel that all they do in the early days is feed!
- In addition, the breastfeeding technique can take a bit of practice to get right. Mums need to experiment with different holds and find solutions for attachment and positioning issues.
- There are potential physiological challenges, such as sore/cracked nipples, breast engorgement, blocked ducts, and mastitis/abscess which mums may have to navigate.
- Feeling like there is not enough milk can be a significant challenge for many mothers in their breastfeeding journeys. However, as I have written about in a previous article, this is mostly a perception issue. In as many as 95% of cases, it is easily surmountable with the proper support.
How important is it to have a supportive community?
I cannot stress enough the huge role a supportive community plays in successful outcomes for breastfeeding. In “the fourth trimester”, women adjust to being mothers just as much as their babies adapt to life outside the womb. This postnatal period seems to be universally defined as 40 days.
Kimberly Ann Johnson, author of the book “The Fourth Trimester” says:
“Everything that a new baby needs, a new mom needs. So you know a new baby needs swaddling, you know a new baby needs a constant food source, you know a new baby needs eye contact, you know a new baby needs soothing. That’s everything a new mom needs.”
But the best way of caring for a breastfed baby is to care for their mother. Feed her, love her, support her by taking care of other stuff. Do housework, run errands, look after older children. The same goes for supporting women who are bottle feeding.
How can we as a society make breastfeeding easier for mothers?
As a society we can further encourage breastfeeding mothers when it comes to feeding in public. Public bathrooms are not acceptable places to feed infants! Establishments can train their staff on how to respond compassionately to a mother whose infant needs to feed, and to take a step further to provide a private space in which to do this, if required. Far too often this is left to the discretion of the staff, and so mothers have mixed experiences. Just one negative experience can be a huge setback to a mother’s breastfeeding journey, making her feel that she has to stop breastfeeding in order to leave the house and ‘have a life’.
Alongside all of this, the government MUST step up and make things easier for new families. In 2018, a significant amendment to the Shop and Office Act was passed in Sri Lanka which mandated the “provision of nursing intervals for nursing mothers” (previously only mandated in the state sector, although sometimes practiced informally in the private sector). This means that working mothers are now entitled to 2 paid feeding breaks of 1 hour per working day until their child is 1 year old.
This is a significant step forward – however longer, better paid leave for both mothers and fathers, as per the Swedish model, would do wonders for the well-being of the whole family, and in increasing breastfeeding figures.
If you are a new mum and are having trouble breastfeeding, you can speak to a doctor on oDoc. You can video call them from your home, baby in hand, even while breastfeeding! You can download the app here.
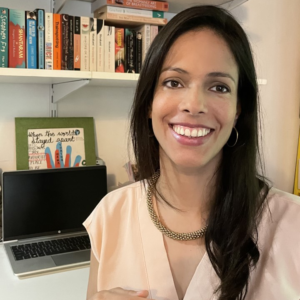
HOW I BECAME ‘THE MILK COACH’
When my first child was born, I was quite unprepared for what lay ahead. Particularly when it came to breastfeeding… I was naïvely expectant that I could just place him onto my chest, and let nature take its course. What a surprise I was in for! Cracked nipples from sub-optimal positioning, and my milk taking its own sweet time to come in, led to terrible pain. This pain became excruciating when my son developed oral thrush which travelled into my milk ducts. Fortunately, thanks to a lot of research and some wise mummy friends, I was able to power through the awful first few months. Most crucially, I was able to advocate for myself with health professionals, when the ‘system’ didn’t really support me.
This birthed a passion to counsel, support and advocate for my fellow Sri Lankan mums. To this end I am working to add to a science background (in Molecular Cell Biology) with an accreditation by La Leche League International (LLLI). My heart is to help YOU to achieve your breastfeeding goals – whether that is one week, one month, six months, or even a year and beyond.
Join the conversation, follow @themilkcoach on Instagram or Facebook.
Similar Articles...

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of

All you need to know about Gestational Diabetes
Did you know that gestational diabetes mellitus, also known as GMD, is one of the most common medical complications of pregnancy? What is GMD? Why
Endometriosis
Endometriosis No woman looks forward to “that time of the month.” Dealing with nausea, stomach cramps, mood swings, back pains and fatigue, all whilst facing