Menopause: The Great Ending of The Menstrual Cycle

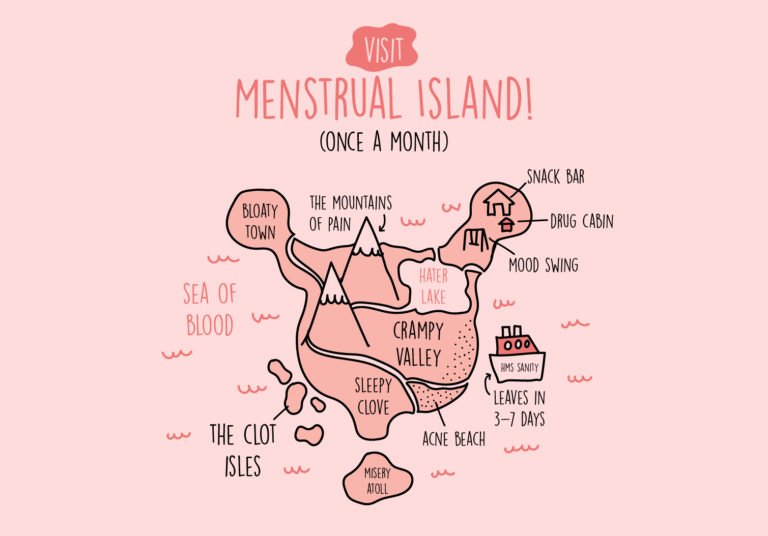
The menstrual cycle – the epitome of the reproductive cycle, which gives birth to life and plays a significant role in the transition from girlhood to womanhood, is considered nature’s phenomenon, gifted to women (minus the agonising PMS symptoms, of course). And after decades and decades of operating the same painful cycle every month, a woman’s menstrual cycle decides to retire into solitude in the mature years of her life.. (great news, right?!)
But do you know what really happens in this ending stage of a woman’s menstrual cycle?
This week’s blog unravels the grand (or rather, long-served) ending of this extraordinary cycle: ‘Menopause’. Keep reading as we explain each stage of menopause and how you can prepare for it.
What is menopause?
As the word suggests, menopause involves the permanent pause of a woman’s menstrual cycle. It is the period that indicates the end of a woman’s menstrual cycle, where usually, if a woman has gone 12 months without her menstrual period, she is said to be having her ‘menopause’.
When does menopause occur in a woman’s life?
It usually occurs between the ages 40 and 50.
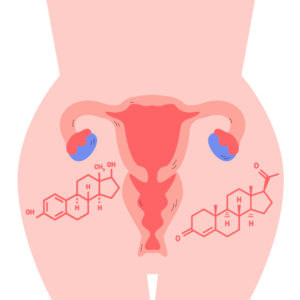
The female sex hormones - partners in crime
Before we dive in deeper, it’s important to know the two main female sex hormones- oestrogen and progesterone. Oestrogen is responsible for the development of secondary sexual characteristics in a young woman and functions such as menstruation, ovulation and pregnancy. Similarly, progesterone also plays an equally significant role in the menstrual cycle, ovulation and pregnancy. They are indeed two hormones tirelessly working hand in hand in a woman’s body!
The stages of menopause
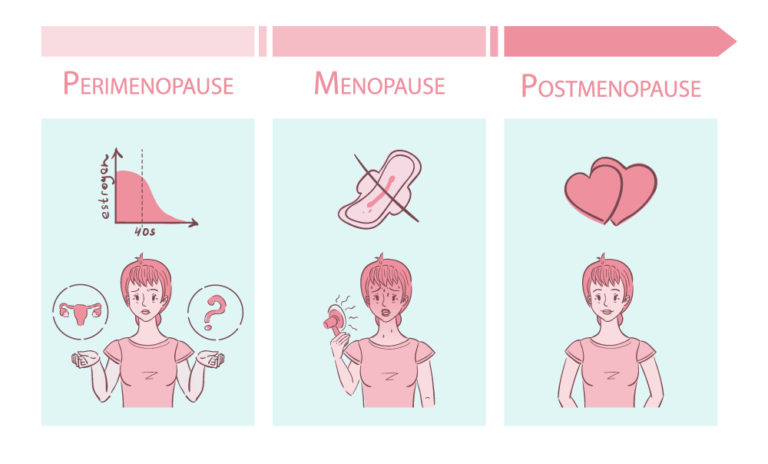
- Perimenopause
This is the first stage that leads up to menopause. Perimenopause is the period in which a woman’s body makes the transition from having an active menstrual cycle to menopause (menopausal transition). Several changes in hormonal levels occur. In this stage, oestrogen levels begin to rise and fall unproportionately. Furthermore, menstrual cycles may either increase or decrease, causing irregular periods. Women may also have menstrual cycles despite ovaries not releasing an egg (ovulation). During this stage, it is possible for symptoms related to menopause, like hot flashes, vaginal dryness, etc., to be present.
- Menopause
Menopause occurs when the female body stops producing the hormones that cause menstrual cycles. These hormones include oestrogen, progesterone, luteinizing hormone and follicle-stimulating hormone. A woman would then not get her period for 12 months consecutively.
3. Post-menopause
This is the final stage of menopause in which a woman hasn’t experienced her period for over 12 months. The body produces significantly fewer amounts of hormones (oestrogen and progesterone), and women will no longer experience a monthly period nor can get pregnant for the rest of their lives. During this stage, the symptoms of menopause may linger around; however, they are less intense.
Symptoms of perimenopause and menopause
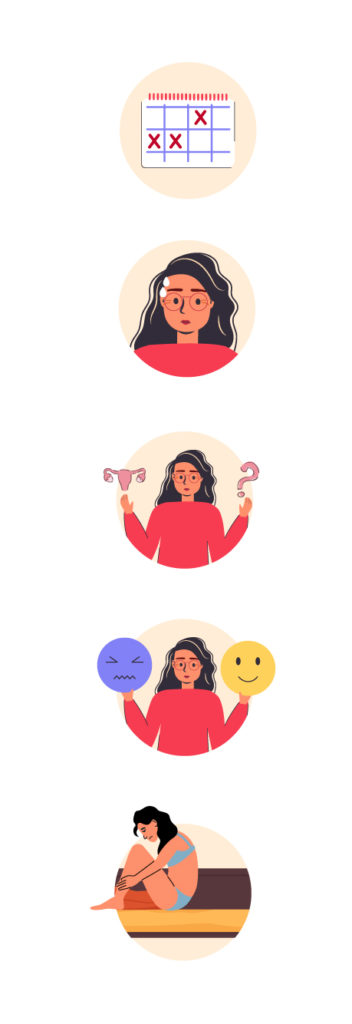
- Irregular periods
Due to hormonal changes in the perimenopause stage, the duration of time between periods may become longer or shorter. Also, period flows may range from light to heavy, while missing periods are common.
- Hot flashes and sleep problems
A hot flash is the sudden feeling of warmth in the upper body. These intense feelings spread over the face, neck and chest areas and skin may redden, causing sweating as well. Often, hot flashes may happen at night, causing inconvenience during sleep.
- Decreased fertility
During the menopausal period, a woman’s ovulation starts to become irregular. This decreases the ability to conceive. Although, it’s important to note that it’s still possible for a woman going through perimenopause to get pregnant, therefore if you are a woman suspecting that you are going through perimenopause and still have your periods regularly, it is advisable to use birth control until you haven’t got your period for more than 12 months.
- Mood changes
A woman may undergo several mood swings, irritability and an increased risk of depression during the perimenopausal period.
- Changes in sexual function/libido
As a woman’s testosterone and estrogen levels drop, it becomes more difficult for her to get aroused, and this causes issues with libido and sexual drive.
Other symptoms
- Loss of bone – Calcium deficiency in bones
- Vaginal and bladder problems
- Increased hair growth on areas such as the face, chest, neck
Not having it with menopause? Fret no more, we give you healthy tips to make this period in your life easier below!
Lifestyle changes for better management of menopause
Menopause is a natural process that all women experience once their reproductive cycles reach maturity, and it may be an uncomfortable experience for most women. However, here are some methods in which the symptoms of menopause can be controlled better to reduce its discomfort.
- Consume foods rich in vitamin D and calcium
Vitamin D and calcium have proved to improve bone health. As a woman undergoes menopause, hormonal changes result in the weakening of bones, increasing the risk of osteoporosis. Foods like yoghurt, milk, fish and eggs are good sources of these nutrients.
- Maintain a moderate/healthy weight
During the menopause period, hormonal changes, aging and lifestyle causes weight gain. This would increase the risk of cholesterol and diabetes.
- Exercise regularly
Exercise and work out sessions have been proven to improve sleep and mental health of menopausal women. Therefore, regular exercise may subside the sleep issues menopausal women undergo.
- Ensure a consistent intake of a protein-rich diet
Proteins help reduce muscle loss and increase overall body strength in women experiencing menopause.
- Consume foods abundant in phytoestrogens such as soya beans, tofu, flaxseeds
Phytoestrogens are a source of dietary oestrogen from naturally occurring plant compounds that have the same function as oestrogen in human bodies. Thus, phytoestrogens may play a vital role in hormonal balance during menopause and reduce symptoms like hot flashes.
When to see a doctor
It is advisable to meet with a gynaecologist if you experience
- Vaginal bleeding after not having a period for 12 months
- Recurring or chronic urinary tract infections (UTIs)
- Bleeding after sex
- Abdominal pain
These signs may indicate more serious underlying medical conditions that need to be diagnosed to begin early treatment. Every woman’s menopausal period is unique and different to one another. If you are experiencing difficulty managing your uncomfortable menopause symptoms, the SLMC-registered gynaecologists on oDoc will help you navigate them, providing improved health and well-being.
Sources
- Menopause – Symptoms and Causes, Mayo Clinic (2020)
- Perimenopause – Symptoms and Causes, Mayo Clinic (2021)
- 11 Natural Remedies for Menopause Relief, Healthline (2022)
- Menopause, The University of Utah (2022)
- Bleeding after menopause: Is it normal? Mayo Clinic (2020)
Similar Articles...

Let’s talk flu, its prevention and home remedies.
Boo-ger season is here! Let’s begin by defining flu (short term for influenza) because it’s usually misunderstood as fever or cold. Flu is a common

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of
How to Keep Work Stress from Taking Over Your Life
How to Keep Work Stress from Taking Over Your Life In today’s fast-paced and competitive world, work stress has become an all-too-common problem that affects