What Goes Wrong in Sleep? An Overview of Sleep Disorders
Consultant Respiratory Physician (MBBS, MD Medicine, MRCP UK, ESRS/ Expert Somnologist)
Good sleep is essential for a good life, and we spend about one-third of our lives sleeping. Therefore, it is essential to be aware of disorders that can occur during sleep, how to identify them, and treatments are available for them.
What types of sleep disorders are there?
There are many types of sleep disorders but here are some of the most common ones:
- Insomnia (difficulty in falling asleep and/or staying asleep)
- Sleep related breathing disorders (eg. Sleep apnoea)
- Central disorders of hypersomnolence (conditions with excessive sleep)
- Parasomnias (involves unusual and undesirable physical events or experiences that disrupt your sleep)
- Sleep-related movement disorders
Let’s take a deeper look into each of the above-mentioned sleep disorders including how each affects the patient and what they can do to prevent them.

Insomnia
People with insomnia find it very difficult to fall asleep and/or sleep well at night despite having a suitable environment and time to sleep. This will result in an impairment in their daytime functioning. In some people, this can be short-term, such as in anticipation of a stressful event like facing an exam or starting a new job. In others, this goes on for many months and years, causing distress to the patient.
Patients with insomnia will be evaluated using
- Sleep diaries – These let you measure and record when the patient went to bed, when they woke up during the night and woke up in the morning
- Actigraphy – It is a wearable sleep test that tracks the patient’s movements while they are sleeping to analyse when they’re asleep and awake
- Polysomnography (sleep study) – It is a comprehensive test that records brain waves, oxygen level in blood, heart rate, breathing, leg movements, etc during the sleep study.
This condition’s management includes sleep hygiene measures, medication revision and cognitive behavioural therapy.
Sleep-related Breathing Disorders
These conditions are involved with abnormal and difficult respiration during sleep. While some of these sleep-related breathing disorders have low health impacts, others may have serious consequences due to their effects on the patient’s sleep and balance of oxygen and carbon dioxide in their blood.
There are a few types of sleep-related breathing disorders. They are
- Obstructive sleep apnoea
- Central sleep apnoea
- Sleep-related hypoventilation disorders
- Sleep-related hypoxemia
Some risk factors of obstructive sleep apnoea are
- Male sex
- Ageing
- Obesity
- Smoking
- Alcohol use
- Certain craniofacial features such as receding jaw or small chin
- Patients or their bed partners complain of loud snoring
- Fragmented sleep
- Getting up frequently to go to the toilet
- Feeling excessively sleepy in the daytime
- Feeling irritable and moody in the daytime

Apnoeic Spells and its Treatments
Sometimes a spouse may notice that the patient stops breathing at night for prolonged periods. This phenomenon is known as an apnoeic spell. Patients are evaluated with sleep studies called ‘polysomnography’, tests that evaluate sleep in detail and diagnose the underlying sleep disorder. The first line treatment is CPAP therapy (a device that provides continuous positive airway pressure). Additionally, weight loss with exercise and a healthy diet are also substantial.
Central Disorders of Hypersomnolence
These are a rare group of sleep disorders where patients complain that they are always sleepy during the day and the night. Patients tend to fall asleep in the daytime even after adequate sleep. E.g. Narcolepsy. Some patients with excessive sleepiness may have an underlying undetected medical or psychiatric condition.
Excessive sleep has a significant detrimental impact on the patient’s life. These patients must be evaluated with sleep studies and blood investigations before starting their treatment.
Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders are a group of disorders where the patient’s body’s clock, which helps to maintain a regular day and night pattern, is affected.
There are several types of circadian rhythm sleep-wake disorders.
- Delayed sleep-wake phase disorder
This is where the patient does not fall asleep until the morning and tends to wake up in the afternoon – the patient’s circadian clock is delayed compared to the average population. These patients may struggle to wake up on time for school and work.
- Advance sleep-wake phase disorder
On the other hand, this disorder tends to have an early sleep pattern and early rise pattern. There are various types of disorders. Shift workers also suffer from the detrimental effects of not sleeping on time and staying awake when they should be sleeping.
- Jet lag disorder
This is another condition in which people suffer due to crossing time zones. Understanding these conditions is vital as many treatment modalities help reduce these problems.
Parasomnias
Parasomnias are another set of sleep disorders involving a lot of sleep movement. In certain sleep stages, some people have confusional arousals, sleepwalking, sleep terrors, sleep-related eating, violent movements in sleep, acting out dreams, nightmares etc. Patients are evaluated with a sleep diary and polysomnography. These conditions must be identified and treated as many patients suffer from poor sleep and daytime dysfunction due to these issues.
Sleep-related Movement Disorders
Sleep-related movement disorders include restless leg syndrome and periodic limb movement disorder, where the patient has a lot of leg movement at night, leading to disturbed sleep.
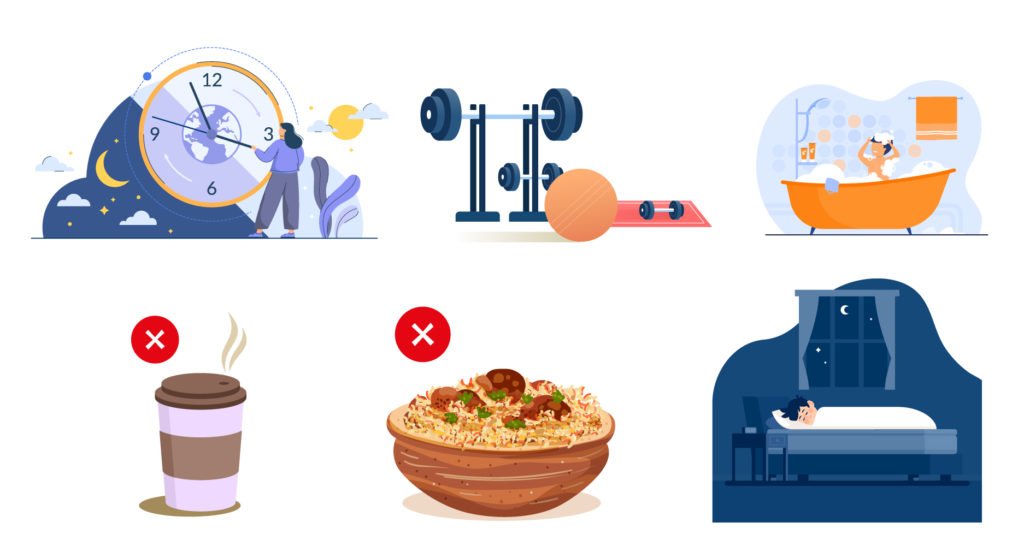
How do you prevent sleep disorders from occurring in the first instance?
The baseline management of any sleep disorder is the maintenance of good sleep hygiene practices.
- Maintain a regular sleeping and waking up time
- Have regular meals
- Avoid caffeinated drinks close to bedtime
- Avoid smoking and alcohol
- Keep your devices away at least one hour before bedtime
Despite these measures, if a patient feels that they have an issue with their sleep, it is best not to delay diagnosis, as sleep is essential for a healthy life. They can consult experienced sleep specialists via the oDoc app to have a comfortable and convenient consultation in just three taps within the comfort of their own home.

Dr Ruwanthi Jayasekara
SLMC 25147
Chest Physician
Sources
- How Is Actigraphy Used to Evaluate Sleep, Sleep Foundation (2022)
- Sleep-Related Breathing Disorders, Sleep Foundation (2022)
Similar Articles...

Let’s talk flu, its prevention and home remedies.
Boo-ger season is here! Let’s begin by defining flu (short term for influenza) because it’s usually misunderstood as fever or cold. Flu is a common

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of
How to Keep Work Stress from Taking Over Your Life
How to Keep Work Stress from Taking Over Your Life In today’s fast-paced and competitive world, work stress has become an all-too-common problem that affects