Understanding Borderline Personality Disorder: Symptoms, Causes, and Treatment.
Borderline Personality Disorder (BPD) is a mental health disorder characterised by instability in mood, behaviour, and relationships. People with BPD experience intense and frequent mood swings, and their self-image and interpersonal relationships are often unstable and erratic. This article will discuss the symptoms, causes, diagnosis, and treatment of Borderline Personality Disorder.
Symptoms of Borderline Personality Disorder
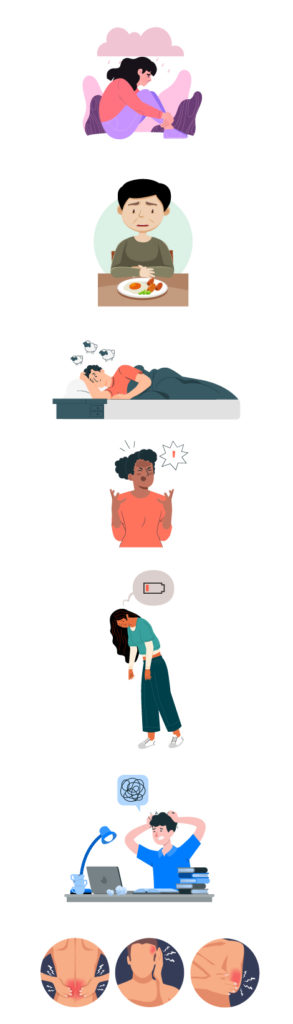
The symptoms of BPD can vary, but they often include emotional instability, impulsive behaviour, fear of abandonment, and an unstable self-image. People with BPD may also have difficulty managing anger, suffer from anxiety and depression, and engage in self-destructive behaviours such as substance abuse, gambling, and risky sexual behaviour.
Individuals with BPD often experience a deep fear of abandonment and may go to great lengths to avoid being alone. This fear of abandonment can manifest in various ways, including clinginess, desperation, or anger when their loved ones don’t meet their expectations. In addition, individuals with BPD often have a distorted self-image and may feel they don’t know who they are. They may change their goals, values, and opinions frequently and have difficulty maintaining stable relationships.


Causes of Borderline Personality Disorder
The exact causes of BPD are not well understood, but it is believed that a combination of biological and environmental factors can contribute to the development of the disorder. Some research suggests that genetic factors may be involved, as individuals with a family history of BPD are likely to develop the condition. Other potential risk factors for BPD include early trauma, neglect, and emotional or physical abuse.
Diagnosis and Treatment
Diagnosing BPD can be challenging, as the symptoms can overlap with other mental health disorders. However, mental health professionals use specific diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) to diagnose. In addition to clinical evaluation, screening tools such as the McLean Screening Instrument for Borderline Personality Disorder and the Personality Assessment Inventory are commonly used to assess BPD symptoms.
There is no known cure for BPD, but treatment can help individuals manage their symptoms and improve their quality of life. Treatment typically involves a combination of medication and psychotherapy. Antidepressants, mood stabilisers, and antipsychotics may be prescribed to help manage symptoms such as anxiety, depression, and mood swings. Psychotherapy, such as Cognitive Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT), can help individuals learn coping skills, emotional regulation, and interpersonal skills.
DBT is a specific type of psychotherapy that was developed specifically for individuals with BPD. DBT focuses on mindfulness, distress tolerance, emotional regulation, and interpersonal effectiveness. This type of therapy has been shown to be effective in reducing suicidal behavior, self-harm, and hospitalizations.

Living with someone with Borderline Personality Disorder
Living with someone who has BPD can be challenging. It is important to remember that the symptoms of BPD are not a personal attack on you, and it is essential to maintain healthy boundaries and take care of yourself. Supporting someone with BPD may involve setting limits, being patient, and encouraging them to seek professional help.
Caregivers of individuals with BPD may also benefit from therapy and support groups. It is important to remember that you are not alone, and there are resources available to help you cope.
Borderline Personality Disorder can be a challenging disorder to live with, but with proper treatment and support, individuals with BPD can lead fulfilling lives. The key to managing BPD symptoms is to seek professional help and engage in therapy. Medication can also help to manage symptoms such as depression and anxiety. It is essential for caregivers and loved ones to be patient and supportive and to seek their own support when needed.
If you or someone you know is experiencing symptoms of borderline personality disorder (BPD), you can start by consulting a psychiatrist or a clinical psychologist from the comfort of your home via the oDoc app.
Sources
BPD: Understanding the Symptomatology – Asian Bio Reviews. https://asianbioethicsreview.com/bpd-understanding-the-symptomatology/
Borderline personality disorder – Symptoms and causes – Mayo Clinic https://www.mayoclinic.org/diseases-conditions/borderline-personality-disorder/symptoms-causes/syc-20370237
Borderline Personality Disorder: How I Learned to Live. – Healthline https://www.healthline.com/health/mental-health/its-not-easy-but-its-possible-how-ive-learned-to-live-with-borderline-personality-disorder