All About REM Sleep and Why it’s Important for your Health
If you are waking up with vivid dreams that you hardly recall, it’s a good sign. Now, for years, it’s a known fact that not getting enough sleep can lead to heart diseases, risk of dementia and even early death. Right now, there are studies confirming that a phenomenon called REM Sleep can be very beneficial for you. Because that affects how you respond to stressful situations, which in turn impacts your physical health. A full circle, yes. So, what is the meaning of REM Sleep? Let’s break it all down for you.
What is REM Sleep?
Ever seen babies with their eyes rapidly moving? It was in the 1950s, the scientists noticed that mannerism and coined the term ‘Rapid Eye Movement’ (REM) Sleep. If that’s a little too unfamiliar, REM sleep is also known as active sleep, desynchronized sleep and dream sleep. REM is one of the stages of sleep during which you dream. In addition to that, it plays a great role in strengthening your memory and improving your brain in many ways.
The research, published in the Journal of Neuroscience, discovered that those who experienced REM sleep had lower fear-related brain activity when given mild electric shocks the next day. This meant that people with REM Sleep are less prone to Post Traumatic Stress Disorder (PTSD).
REM Sleep usually occurs 90 minutes after you fall asleep. During that period, your heart rate and breathing increases. And there will be a very high brain activity which will lead you towards having intense dreams.
Remember, this is a normal and healthy cycle of sleep that you should experience regularly. Therefore, we are going to give you a little more insight to understand how dream sleep can be a game changer.

How Do You Experience REM Sleep?
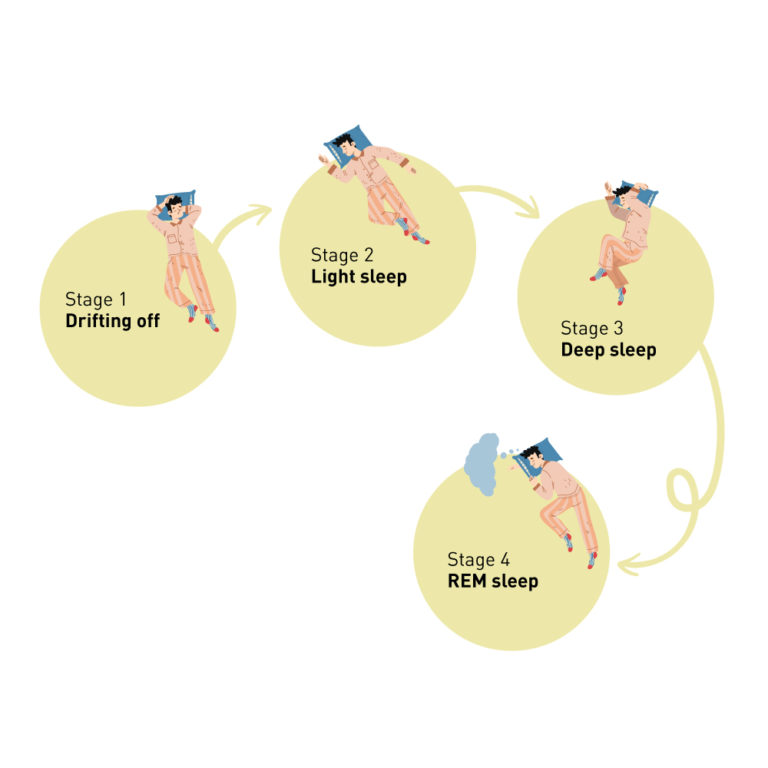
To be aware of what your brain and body experiences during REM Sleep, it’s important to know the stages of sleep.
During a full night’s sleep, you go through all the stages of sleep multiple times. Each cycle takes about 90-120 minutes to complete. With every new cycle, you will spend more time in the REM sleep stage. Let’s say your sleep gets interrupted, you start all over again.
- Stage 1 (Drifting off): Your brain waves, heartbeat, breathing and eye movements all slow down. Then, your muscles start to relax with random twitches.
- Stage 2 (Light Sleep): Your heart rate and body slow down further. Your temperature drops and eye movement stops. You begin to experience sleep spindles and K-complexes, these cause an outburst of activities in your brain.
- Stage 3 (Deep Sleep): Your brain functions at its slowest helping your body to relax your way into deep sleep. Waking up someone at this stage is not very easy. Did you know at this stage your body repairs itself, boosts your immune system and restores your bones, muscles, and tissues?
- Stage 4 (REM Sleep): The brain activity here is similar to how it functions when you are awake. You experience a loss of muscle tone, except for your eyes, that will move rapidly. Researchers have theorized that this happens to protect you from acting out your dreams and injuring yourself.
So, Why Do You Dream During REM Sleep?
As mentioned a little earlier, your heart rate increases and your brain activity is enhanced. Therefore, you tend to experience vivid and intense dreams. To add to that, there is heightened activity in visual, motor, emotional and autobiographical memory parts of your brain. So the areas such as the ones that control rational thoughts are still very slow. Therefore, your dreaming experience doesn’t fully make sense until you wake up and realize it’s just a dream.
Scientists believe that dreams are like a data dump that is gathered through all our experiences so it can act as a second gut.
Benefits of REM Sleep
Dreaming
Some sleep experts call dreaming as an overnight therapy. It prepares you for adverse experiences and this is why those with good sleep react better to bad news.
Emotional Stability
Ever wondered why you feel a bit too sensitive on days when you don’t get enough sleep? This is because sleep regulates your emotions, there is a dedicated brain region called amygdala to process your emotions. And that activates during REM sleep. Again, your vivid dreams also play a major role in this.
Better Memory
During REM sleep, your brain manages new learnings and motor skills from the very day. Some of these are added to memory and some are simply deleted off.
Brain Development
According to studies, REM sleep plays a huge role in brain development. This is why it’s believed that babies spend 50% of their sleep in REM while adults are left with 20% of this sleep.
Waking Up Fresh
If you have a complete night’s sleep, it’s easy to wake up, isn’t it? This is because REM sleep activates your central nervous system.
What happens if you don’t have enough REM sleep?
- You could experience forgetfulness and have poor memory as your brain is deprived of memory growth which occurs during REM sleep.
- Excessive daytime sleepiness. This will lead to many issues including unproductive lifestyle and therefore, sadness.
- Difficulties with concentration. You will observe a downward pattern of your cognitive performance.
- Chronic sleep deprivation or insomnia leads to diabetes, depression, obesity, etc.
Ways to Get REM Sleep
- Sleep in a cool, dark room.
- Go to bed at night around the same time.
- Power down the electronics.
- Relax your body with either meditation or the use of calming mists, etc.
- Avoid regular consumption of alcohol, drugs and nicotine.
- Stay away from artificial light.
- Don’t overly depend on alarm clocks. And use it as a last resort. When your sleep schedule is in sync with your body, you can be up before your don’t-get-too-late alarm bell goes off. This is because multiple alarms can hinder the completion of your strongest REM sleep.
When should you go to a doctor?
If you’re feeling a bit sleep deprived or feel the effects of insomnia, consult your doctor. Also, there are REM-related sleep disorders. So, if your vivid dreams get a bit too scary, if you experience sudden loss of muscle tone during the day, sleep paralysis or have trouble breathing during sleep, get medical attention as soon as possible.
With oDoc, your doctor’s appointment is faster and most effective. You can get in touch with the country’s leading GPs over a call. So, convenient that you don’t have to lose sleep over it.
Sources
- Cleveland Clinic
- Sleep Foundation
Similar Articles...

Let’s talk flu, its prevention and home remedies.
Boo-ger season is here! Let’s begin by defining flu (short term for influenza) because it’s usually misunderstood as fever or cold. Flu is a common

Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment
Menopause Brain Fog is real: A Simple Guide with Symptoms and Treatment Women in their 40s and 50s who are just entering the end of
How to Keep Work Stress from Taking Over Your Life
How to Keep Work Stress from Taking Over Your Life In today’s fast-paced and competitive world, work stress has become an all-too-common problem that affects